Fitwits was created by Kristin Hughes, a communication designer at Carnegie Mellon University. The program did not begin with a big vision to impact the eating habits and health of children and their care-givers — it started with one small assignment to observe a badly failing online approach intended to entice kids to record their own food intake. Fitwits grew from Hughes’s insights into the gap in communication between doctors, young patients and their families — when she asked the doctors involved if they used the word obesity during well-child check-ups, they admitted that “talking obesity was challenging.”
The Fitwits program addresses the growing issue of obesity in children, with an emphasis on health and nutrition education as well as on disease prevention.
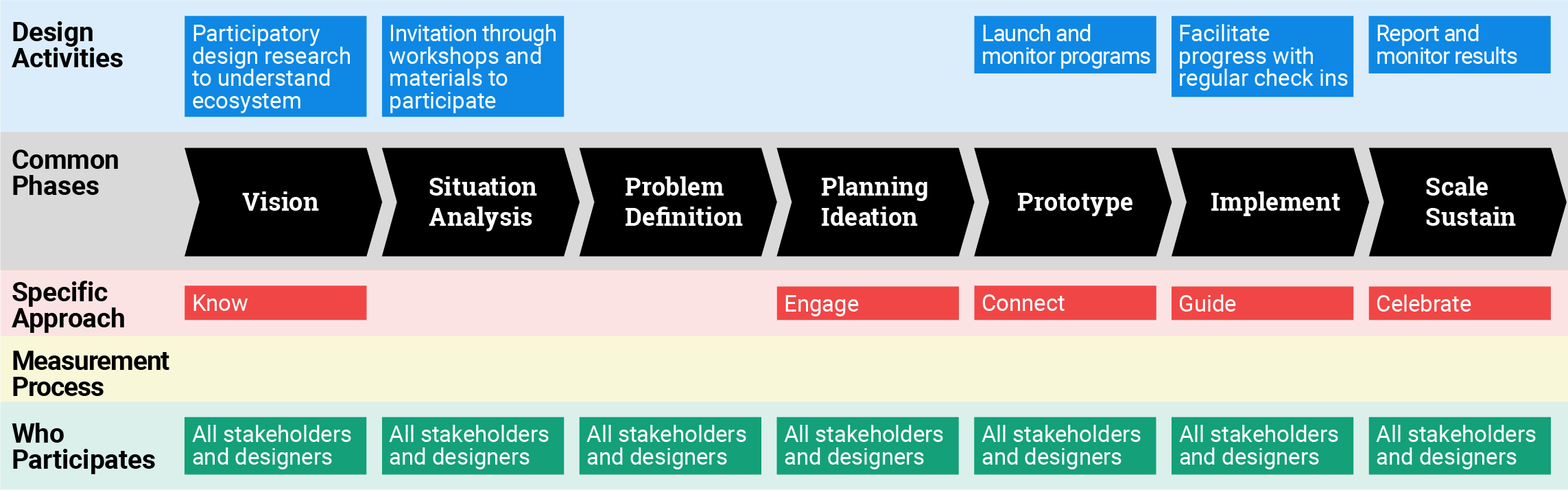
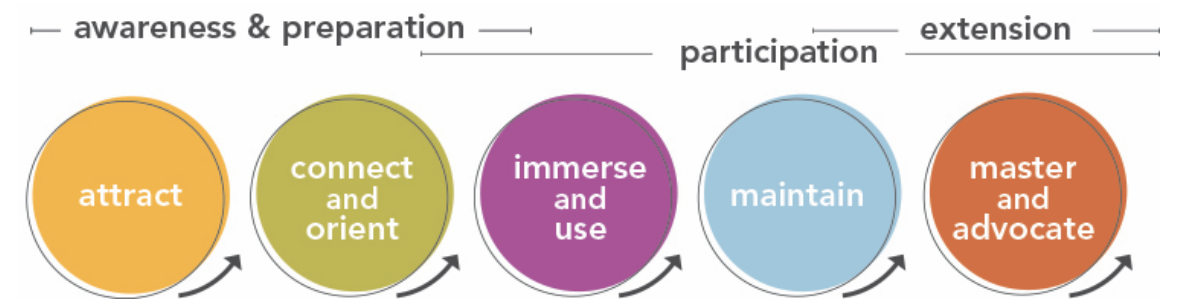
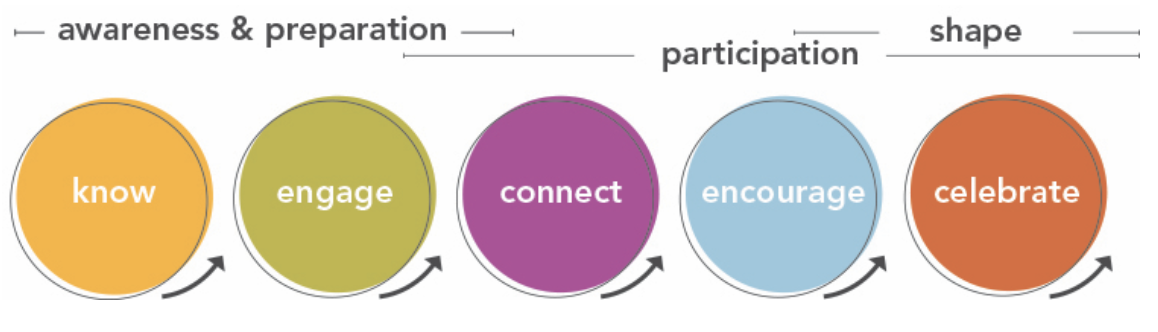
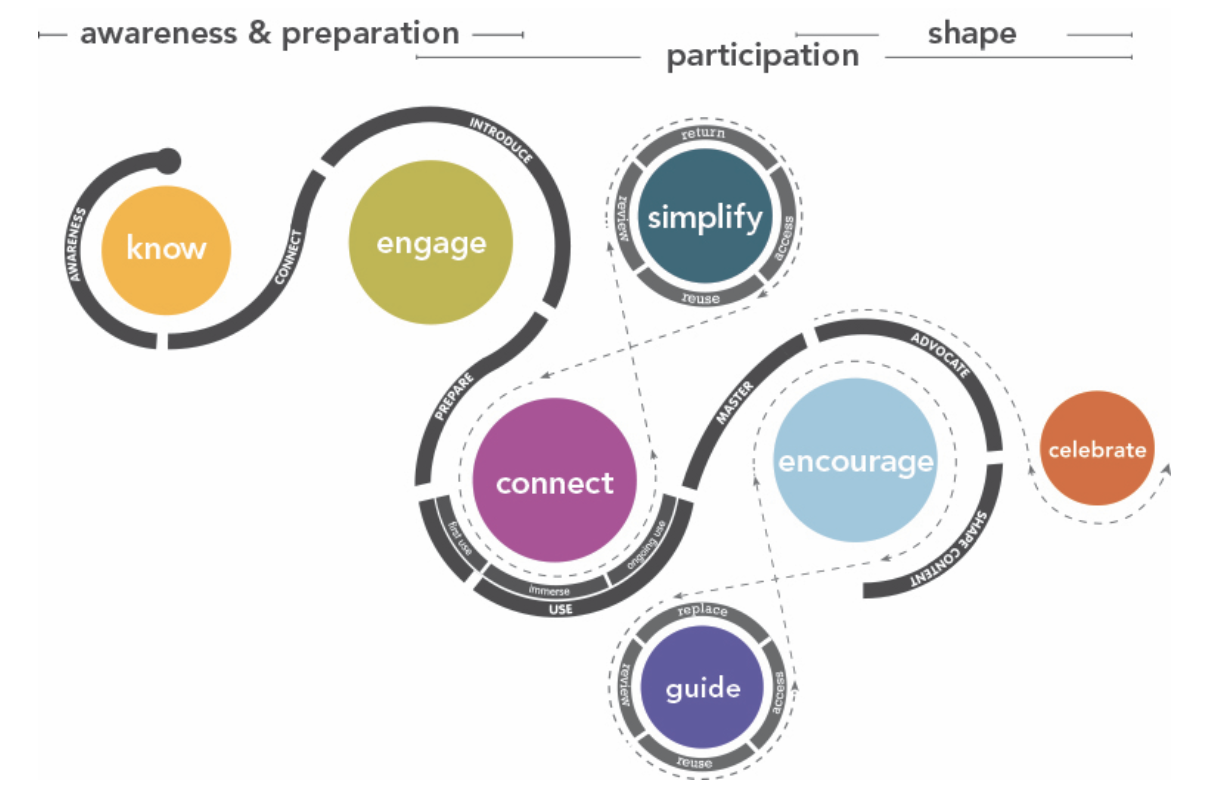
Fitwits provides an interesting solution to the problems described above, largely through a strong emphasis on service design. The service Fitwits offers is multi-fold. First, it is basic nutrition education, made attractive to children through the use of a thoughtfully designed toolkit based on didactic play. The design process employed allowed the team to consider the experiences of its participants first and foremost in its implementation. Participants’ experiences, whether child, doctor, parent, and teacher, were considered with equal levels of attention, with the understanding that engaging these audiences would require a comprehensive communication approach addressing individual learning styles and interests.
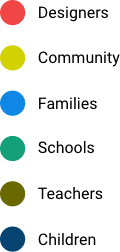
As understanding of the issues grew, the entire team began to map the ecosystem involved in children’s access to and knowledge of food and health. Eventually, Fitwits became what Hughes calls an “ecological model” of social design, wherein a strong emphasis is placed on the confluence of the individual, family, community, and society in approaching public health interventions. For example, the 6-month Fitwits school-based game operates at the various levels where obesity related health decisions are shaped. At the individual level, the game is designed to teach children about nutrition, and increase physical activity. Children received a wristband with tokens added as the child meets challenges, thus increasing and sustaining motivation and play. At the interpersonal family level, challenges were sent home to inform and motivate families to engage in healthy eating and physical activity. At the interpersonal level, classrooms compete with other classrooms keeping teachers and children engaged and motivated. At the organizational level, the Fitwits challenged school administrators to implement policies that encourage healthy nutrition and physical activity (i.e. Nitwit Free Tuesday, a day when Chips and/or soda were not allowed on school grounds). A community scoreboard and “Wall of Champions” in schools encouraged everyone to participate in Fitwits competition.
At the time of its launch in 2007, the program was housed within the Carnegie Mellon University School of Design. Since then, numerous components have been deployed in schools, physicians’ offices, community organizations, restaurants, and homes. All components were successfully piloted in various locations throughout the US and several have been implemented multiple times in different settings—all resulting in changed eating habits. In 2014, when Fitwits left the University, it formed an LLC, but did not secure the funding required to become an independent entity. Key stakeholders are still researching Fitwits in their locations.
Hughes says it was the process of design that made the Fitwits project unique. The products and services were carefully planned with all stakeholders in mind; the system was flexible enough to adapt to diverse and evolving needs; the immersion supported going deep where traditional approaches and time constraints don’t typically allow. Participatory design sessions were carefully planned, often spending weeks alongside the community, getting to know them—carefully co-designing a solution that would work for them. The design team was able to gain empathy and build trust with people who are never asked to be part of the solution.